Hip and knee total joint arthroplasties (TJA) are among the most common surgeries in the United States. Nationally, same-day discharges are becoming increasingly common, and length of stay (LOS) in post-operative rehabilitation has been decreasing.
Hospital for Special Surgery (HSS), the leading academic medical center focused on musculoskeletal health in the United States, has long referred patients to VNS Health after discharge.*,† Because of VNS Health’s expertise in home care and rehabilitation therapy and HSS’s reputation, we were natural partners in a collaboration aimed at improving TJA outcomes (including reducing rehospitalization rates) and decreasing costs.
In 2011, we set out to establish a process for decreasing LOS both in the hospital and in at-home rehabilitation therapy after TJA — the impetus being that shorter LOS in a hospital setting has been found to be associated with improved patient outcomes and experience, as well as lower costs.‡
We recently spotlighted the outcomes of this collaboration in an article published in the February 2024 issue of HSS Journal: The Musculoskeletal Journal of Hospital for Special Surgery. Titled “VNS Health and HSS Partner to Reduce Length of Stay After Total Joint Arthroplasty: Implications for Home Care Providers,” the article was written by Sandy Merlino, Vice President of Business Development, and Joe Gallagher, Director of Operation Support Services.
Outcomes of VNS Health’s Collaboration with HSS
The process we developed has shortened LOS in the hospital and has allowed patients to bypass inpatient rehabilitation and to receive fewer in-home visits from a rehab therapist — all while maintaining or improving patient outcomes and decreasing rehospitalizations. Additionally, shortening LOS in the hospital and allowing patients to be discharged directly home have led to lower costs of care.
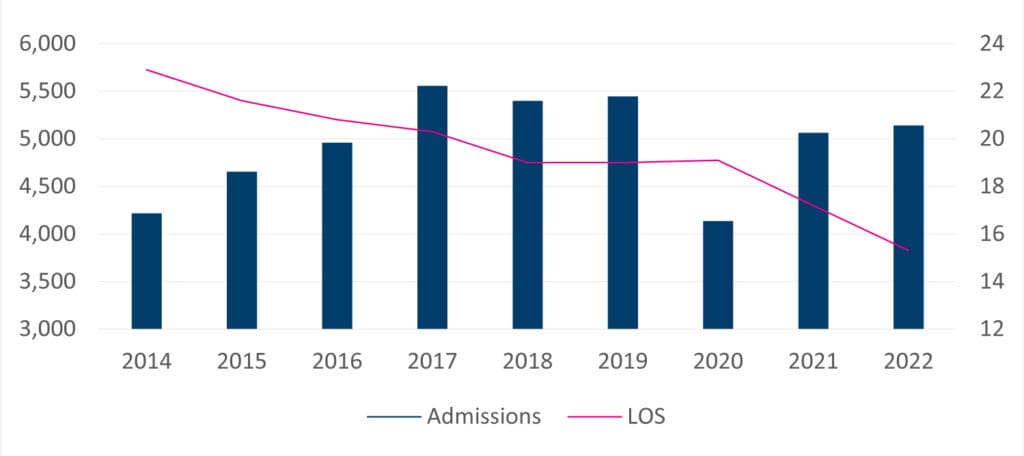
Hospital LOS averaged 3–5 days at the outset of this collaboration, whereas most patients are now discharged within a day of their surgery. Moreover, the average LOS in at-home rehabilitation decreased from about 23 days in 2014 to about 15 days in 2022.*
Our greatest concern was how these changes would affect patient outcomes. We needed to ensure that despite having less-frequent rehabilitation therapy, patients were still recovering from surgery as well as, or better than, they would in an inpatient facility. Safety was also a concern because patients who were discharged home would not have access to round-the-clock nurses to monitor incisions for infection.
Improved Outcome-Based Quality Improvement Metrics
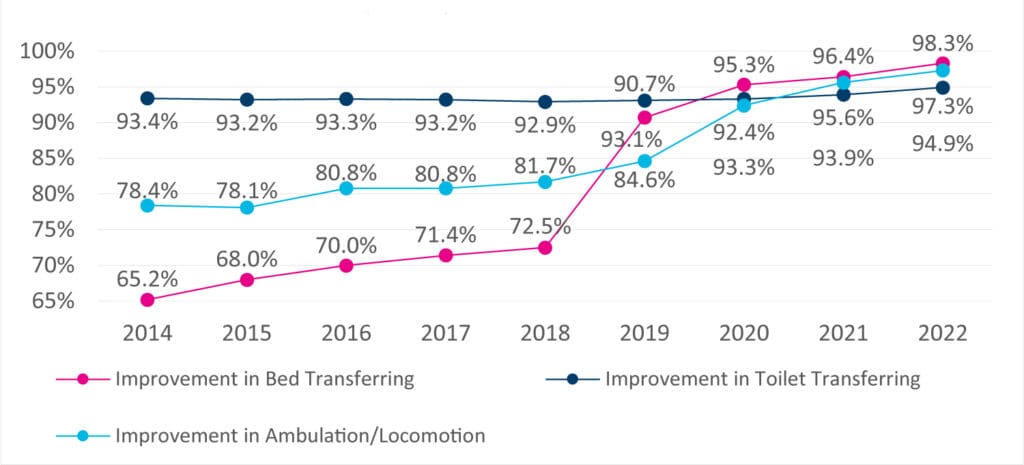
We tracked three quality improvement metrics: toilet transferring, bed transferring, and ambulation/locomotion.
Remarkably, even though patients bypassed inpatient rehabilitation and received fewer in-home visits, patient outcomes generally remained the same, and certain ones improved. In regard to toilet transferring, the percentage of patients who improved from start of care to discharge remained fairly consistent. The percentage of patients who showed improvements in ambulation increased by nearly 25%, and the percentage who improved in bed transferring increased by slightly over 50%.*
Moreover, research from HSS in 2015 revealed no difference in post-operative complications among patients recovering from knee replacement surgery who were discharged to inpatient rehabilitation versus those who were discharged directly home. When it came to function, pain, and overall patient improvement, 2-year outcomes were similar between the two groups.†
VNS Health offers a wide range of health care solutions to help you care for your patients and their needs. Learn more about referring to home care.
Lower Rehospitalization Rates
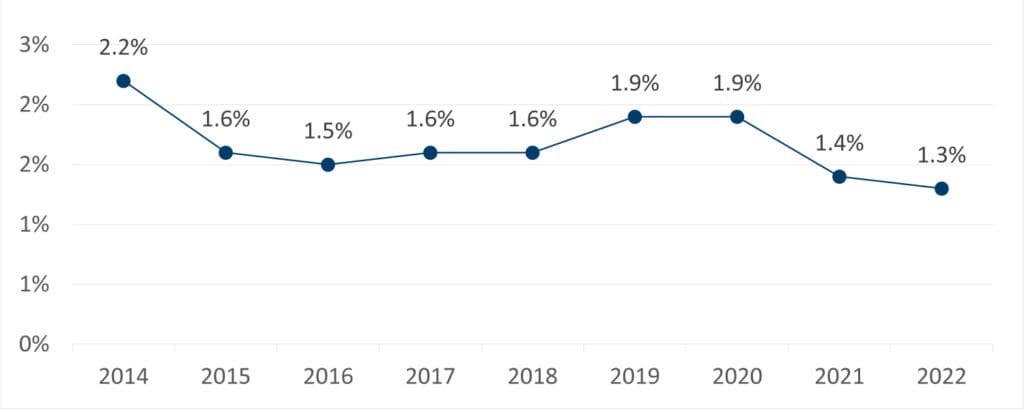
Rehospitalization rate was a critical measure for us to track.
Hospitalized patients are at increased risk for complications (such as falls and health care–associated infections) and, in recent years, for exposure to COVID-19. Furthermore, the hospital environment can be detrimental to patients’ mental well-being and can contribute to their overall dissatisfaction with their care.
Avoiding rehospitalization is essential from a financial perspective as well. Hospitals are responsible for all costs associated with a single TJA episode — costs that can dramatically increase with rehospitalization. This fact has incentivized hospitals and organizations like VNS Health to work together on improving both quality and efficiency.
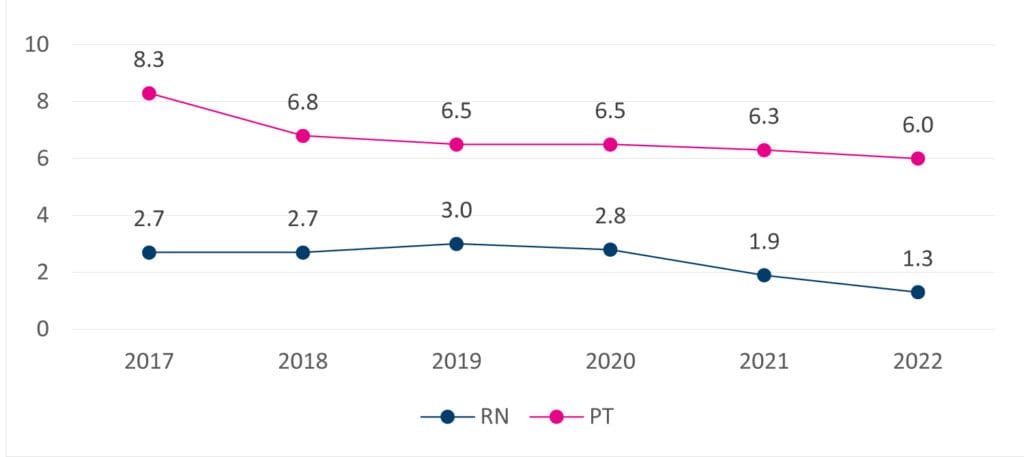
Despite initial concerns that discharging TJA patients early would increase their risk of rehospitalization, we discovered the opposite to be true. As LOS decreased, the percentage of patients who were rehospitalized within 30 days of discharge also decreased, by 41%.*
Factors Contributing to Reduced LOS
LOS in post-operative care can be reduced by decreasing the time spent in the hospital directly after surgery, the time spent in post-discharge rehabilitation, or both. Meeting our goal of reducing post-operative LOS required committing to an early home care visit, adjusting the frequency of at-home rehab, and enhancing communication.
Timely First Home Care Visit to Reduce LOS in Inpatient Facilities
Compared to discharge to inpatient facilities, home discharge may:
- Decrease per-episode costs of care
- Reduce the risk of complications
- Improve patient satisfaction and overall experience
- Decrease rehospitalization rates
- Lower likelihood of post-discharge morbidity
Despite these potential benefits, when we began our initiative to reduce LOS, TJA patients often stayed at HSS for 3–5 days following surgery, and a large percentage were discharged to inpatient or subacute rehabilitation facilities for 1–3 weeks.*
To address this situation, VNS Health committed to conducting an initial home care visit within 24 hours of discharge, and HSS began discharging patients as soon as they were medically and functionally cleared. These practices have allowed patients to be discharged directly home, bypassing inpatient rehabilitation. About half of HSS’s TJA patients now go home on the same day, and the rest generally stay for only one night before discharge.*
Adjusted Frequency of At-Home Rehabilitation and Personalizing Care
Personalized care and efficiency were key in reducing LOS in at-home rehabilitation.*
To ensure that patients were receiving the same quality of care at home as they would in an inpatient setting, we piloted the Intensive Rehab at Home program, whereby patients received a daily physical therapy visit. When Medicare reimbursement models changed in 2016, we assessed whether or not each patient actually required such an intensive rehabilitation regimen.
We found that many patients did not need daily rehabilitative care, as long as their care plans were tailored to their needs and environment. Customizing care in this way decreased the frequency and duration of rehabilitation for many patients — from every day for about 4 weeks to an average of just six visits over a 2-week period.*
We found that the change resulted in maintained or improved outcomes — indicating that patients did not need as frequent rehabilitation, or as much face time with medical staff, to ensure quality recovery and prevent infection and rehospitalization.*
VNS Health also worked with HSS to take advantage of innovations in surgical care — such as rapid recovery protocols for pain management and new anesthesia techniques — by modifying how we provided home care in order to optimize rehabilitation and recovery and thereby decrease LOS in at-home rehabilitation.
For instance, it used to be that surgical dressings could be changed only by a nurse. However, because of the rise of minimally invasive surgeries and the use of surgical glue and atraumatic dressings, like Mepilex, to seal outer wounds (rather than traditional staples and stitches), HSS staff members could instead teach our physical therapists to safely change dressings.
This allowed our physical therapists to work to the top of the license, thereby decreasing the number of providers required for care and increasing the efficiency of individual providers.
VNS Health has the expertise to care for your patients requiring rehab therapy. Contact us to learn more.
Enhanced Communication Between VNS Health and HSS
Communication has been a critical element in optimizing patient outcomes and, ultimately, in the success of our collaboration with HSS. Using a shared, secure, HIPAA-compliant transport layer security tunnel, our organizations can easily communicate with each other, as well as share and view critical patient data in real time.
We also hold weekly meetings with the HSS Center for the Advancement of Value in Musculoskeletal Care, during which we review every patient who is in their 2 weeks of home care. We discuss possible barriers to discharge from home care, ensure alignment between our organizations’ values and visions, and improve clinical pathways and performance.
These meetings have proven invaluable financially. Through the meetings, VNS Health and HSS began collaborating on the management of bundled payment programs and value-based-care initiatives — a collaboration that has contributed to millions of dollars in annual savings.
Summary
Our collaboration with HSS has proven successful. Together, we have been able to reduce LOS both in the hospital and in at-home rehabilitation after TJA, all while maintaining or improving outcomes.
We are looking forward to future collaborations with HSS — whether it’s on further decreasing LOS after surgery and optimizing outcomes or on something entirely new. We are continuing to work as a team toward providing our patients with advanced, optimal, compassionate care.
References
*Gallagher J, Merlino S. VNS Health and the Hospital for Special Surgery partner to reduce length of stay after total joint arthroplasty: Implications for home care providers. HSS Journal. 2024;20(1):117–121. doi:10.1177/15563316231205457.
†Hospital for Special Surgery. Study: Patients who go home after knee replacement do as well as those discharged to rehab facility [press release]. https://www.hss.edu/newsroom_study-patients-who-go-home-after-knee-replacement-do-as-well-as-those-discharged-to-rehab-facility.asp. Published March 24, 2015. Accessed February 7, 2024.
‡Tipton K, Leas BF, Mull NK, Siddique SM, Greysen SR, Lane-Fall MB, et al. Interventions to Decrease Hospital Length of Stay. Agency for Healthcare Research and Quality Publication No. 21-EHC015. https://www.ncbi.nlm.nih.gov/books/NBK574438/. Published September 20, 2021. Accessed February 7, 2024.